In this retrospective study, the orthopaedic team at the Marshall University Joan C. Edwards School of Medicine and Marshall Health performed 25 revision knee replacements with a robotic assisted computer system. The procedure involved placing new implants at the end of the thighbone and top of the shinbone with the computer’s aid to ensure the knee was stable and balanced throughout the range of motion. Researchers then carefully compared the initial positions of the primary implants with the final planned positions of the robotic revision implants for each patient, assessing the differences in millimeters and degrees.
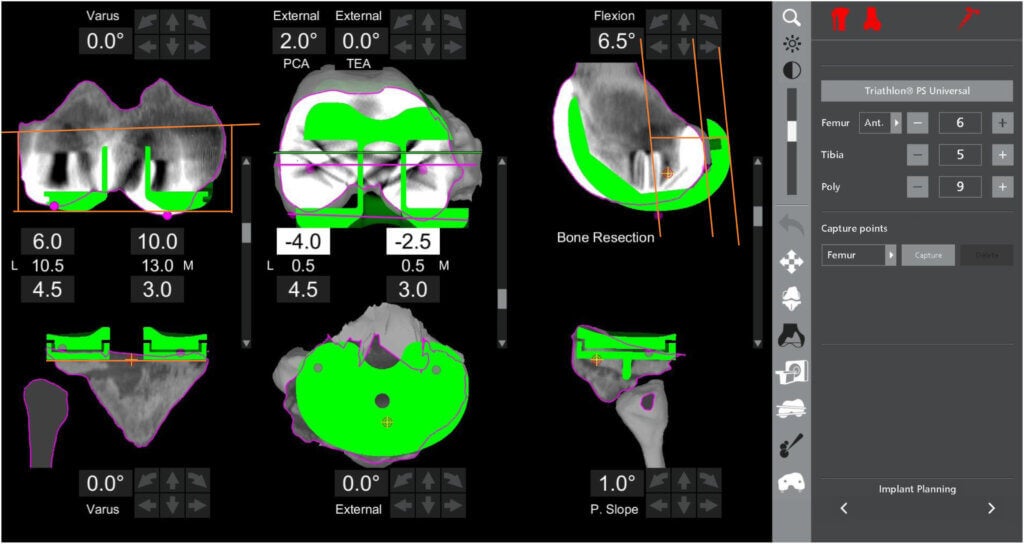
The analysis found that exceedingly small changes in implant position significantly influence the function of the knee replacement. Robotic assistance during revision surgery has the potential to measure these slight differences. In addition, the computer system can help the surgeon predict what size implant to use as well as help to balance the knee for stability.
“Robotic-assisted surgery has the potential to change the way surgeons think about revision knee replacement,” said Matthew Bullock, D.O., associate professor of orthopaedic surgery and co-author on the study. “The precision offered by robotic-assisted surgery not only enhances the surgical process but also holds promise for improved patient outcomes. Besides infection, knee replacements usually fail because they become loose from the bone or because they are unbalanced leading to pain and instability. When this happens patients can have difficulty with activities of daily living such as walking long distances or negotiating stairs.”
The study underscores the importance of aligning the prosthesis during revision surgery. The research also suggests potential advantages, including appropriately sized implants that can impact the ligament tension which is crucial for functional knee revisions.
“These findings open new doors in the realm of revision knee arthroplasty,” said Alexander Caughran, M.D., assistant professor of orthopaedic surgery and co-author on the study. “We continue to collect more data for future studies on patient outcomes after robotic revision knee replacement. We anticipate that further research and technological advancements in the realm of artificial intelligence will continue to shape the landscape of orthopaedic surgery.”
In addition to Bullock and Caughran, co-authors from Marshall University include Micah MacAskill, M.D., resident physician; Richard Peluso, M.D., resident physician; Jonathan Lash, M.D., resident physician; and Timothy Hewett, Ph.D., professor.
To view the article “A Three-dimensional Comparison of Pre- and Post-component Position in a Series of Off-label Robotic-assisted Revision Total Knee Arthroplasties” in its entirety, please visit https://doi.org/10.1016/j.artd.2023.101310.
For more information about the study or for individuals who have a painful knee replacement or are in need of a knee revision, please contact Marshall Orthopaedics at 304-691-1262 to schedule a consultation.
Photo caption: The robotic implant planning page depicts the final position of the robotic revision implant (RRI) in green overlying the primary implants (PI) in white to ensure the best fit for the patient.
###
About the Joan C. Edwards School of Medicine
The Marshall University Joan C. Edwards School of Medicine is a community-based medical school established in 1977. Located in Huntington, West Virginia, the School of Medicine trains physicians, scientists, and other professionals to meet the unique health care needs of rural and underserved communities. Learn more at jcesom.marshall.edu.